Table of Contents
Coronary artery disease is one of the key diseases that we are looking for as cardiologists. It leads to heart attacks, sudden death, heart failure and causes symptoms like chest pain and breathlessness. In this article I explain how we look for it, what we do when we find it, and what the different treatment strategies are. In addition, I have a look at the costs of coronary angiography and coronary angioplasty. I hope you find it useful!
What does heart blockage mean and what problems do heart blockages cause?
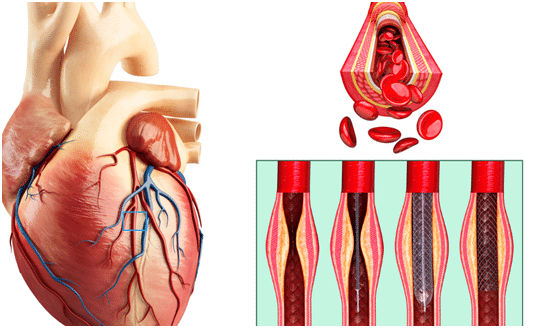
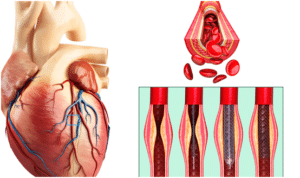
The heart is basically a muscular pump, and its blood is supplied by 3 coronary arteries. As with any artery in the body, these arteries can develop fatty plaques in the walls (atherosclerosis) over time and this can cause 2 main issues:
- Stable coronary artery disease: This is when over time the plaques in the artery walls grow, eventually the blockage begins to obstruct blood flow down the artery. At rest, the heart muscle does not need to much blood so these blockages don’t cause any problems, however at stress or on exertion, the muscle needs more blood and if there is a severe blockage the heart does not get enough oxygen and you feel it as chest pain or dyspnea on exertion (angina).
- Unstable coronary artery disease (heart attacks): The plaques in the walls of the coronary arteries get inflamed and one of them ruptures. This emergency event causes a clot to develop in the artery, stopping blood flow very quickly. This clot is what causes a heart attack and the patient usually experiences sudden onset severe chest pain.
How does your cardiologist assess for blockages?
When you first see your cardiologist, they will ask you about symptoms that can often indicate blockages like chest pain or breathlessness. They will then order some tests to assess for blockages.
- ECG – A simple electrical tracing of the heart, that can pick up signs of many different heart diseases. Takes 15 minutes.
- Echocardiography – A heart ultrasound, that is useful to look for signs of previous heart attacks. Takes 30 minutes.
- Stress test – The patient undertakes some exercise, usually on a treadmill, but can also be done using medication if patient is unable to exercise. The cardiologist looks at the way the heart responds to exercise using ECG and sometimes echocardiography or nuclear imaging. Takes about 30 min to 1 hour.
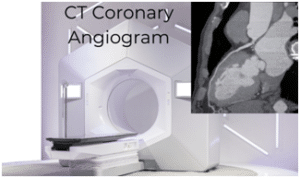
- CT coronary angiogram – This is a CT scan that looks directly at the heart arteries using X-rays. The patient is given an injection of contrast into the veins and the coronary arteries can be directly imaged. Takes about 30min to 1 hour.
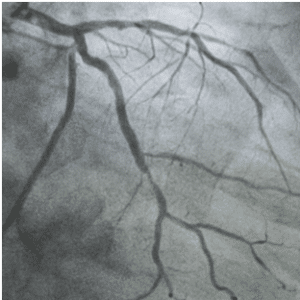
- Invasive Coronary angiogram – This is an invasive test. A catheter is put in the heart arteries and dye is injected, then special X-rays are taken to look for the blockages. It is the gold standard for blockages, however because it is invasive, it has higher risks and is higher cost than the other tests, be sure to talk with your insurance provider if such procedure is included in your coverage. Takes about 30 minutes – 1 hour.
What is the difference between a coronary angiogram and a coronary angioplasty?
A coronary angiogram is done to confirm the diagnosis of coronary artery disease/blockages, whereas an angioplasty is the treatment for the coronary artery disease/blockages.
What happens during a coronary angiogram?
This procedure is the gold standard diagnostic test to confirm coronary artery disease (blockages). It is usually done as a day-case procedure under local anesthetic. You will be asked to fast before the procedure for around 6 hours. Here is an explanation on what will happen to you during the procedure:
- You will initially be admitted to the day ward, where you will see a nurse and your doctor who will explain the procedure, and its risks and ask you to sign a consent form. You will change into a hospital gown.
- When it is your turn you will be taken to the cardiac catheterization lab. You will lie flat on the cardiac catheterisation table and the area where the catheter will be inserted will be cleaned and then draped with surgical covers. The coronary angiogram is usually done through the radial artery in the wrist but sometimes it needs to be done via the femoral artery at the top of the leg.
- An injection of local anesthetic is given at the wrist or the groin and following this a tube (sheath) is inserted into your artery. This allows catheters and wires to be easily put in the artery without bleeding.

- A wire is then passed through the sheath and x-ray images are taken as the wire is pushed up to the aorta at the top of the heart.
- Once the wire is in position a long tube (catheter) is inserted over the wire up to the coronary arteries and the wire is removed.
- Iodine based contrast solution is then injected into the coronary arteries and x-ray pictures are taken from multiple angles to look for blockages.
- If there is no need for angioplasty treatment, the catheter and sheath will be removed, and a device will be used to apply pressure to the artery at the wrist to prevent any bleeding and let the artery heal.
What is a coronary angioplasty?
Coronary angioplasty is the procedure used to treat the blockages if necessary.
- After the coronary angiogram is done, the type of catheter will be changed using a wire and it is positioned at the coronary artery origin.
- A very thin wire will be passed through the catheter, down the coronary artery and past the blockage.
- Once in position a catheter with a very small balloon at the end will be passed over the wire. When over the blockage, this balloon will be inflated with fluid and this opens the blockage.
- When a stent is put in, the same technique is used. The stent is pre-mounted on a balloon and when the balloon is inflated it opens the blockage and the stent squeezes against the wall and holds the artery open.
How do you decide between treating with medication and having an angioplasty?
This is not always a simple decision. We generally decide to treat blockages for 2 main reasons:
- To improve a patient’s prognosis ie prolong life and prevent things like heart attacks and heart failure.
- To improve a patient’s symptoms.
Not all blockages worsen your prognosis, so if they are not causing any symptoms then these types of blockages do not need stented. Several factors need to be weighed before you decide to open a blockage:
- Severity of the blockage: In most cases you need to prove the blockage is severe before you open it. There is no place for doing angioplasty in mild, or moderate disease that is not obstructing blood flow.
- Position of the blockage: Blockages at the proximal part of the coronary arteries are often more significant, and multiple blockages or those involving the left main stem are more likely to be associated with worse long-term prognosis.
- Other conditions: If you are diabetic for example, often a coronary artery bypass graft procedure may be better for you than a stent. Also, if you have another disease that shortens your life expectancy then perhaps you do not need stenting.
- Ability to take blood thinners: When you have a stent put in, you need to take 2 blood thinners together for a few months, this is to stop the stent blocking off with a clot. After this, you need to take one blood thinner like aspirin for life. If you have bleeding issues or cannot take blood thinners for another reason, then maybe stenting is not appropriate for you.
- Symptoms: If you do not get any symptoms from the blockage, then there is no need to stent it unless we think that we can improve your overall prognosis. Note, it is a common misconception but stenting a blockage in stable coronary artery disease, in many cases, does not reduce your risk of a heart attack.
- Heart function: If you have poor heart function this can influence the decision on opening blockages.
- Patient preference: Some patients do not want to undergo open heart surgery, so in these cases, coronary angioplasty can often be offered instead.
Can my artery block again after a stent?
Yes, it can, but it is rare. It is called restenosis.
- In the days before stents, patients would have blockages just opened with a balloon, and the rate of restenosis was 30-50% at 1 year.
- When stents were first introduced, they were called bare metal stents. The rate of restenosis dropped with these stents to about 10-30%.
- Then stent technology involved to have a drug coating that prevented the re-blockage and now the rate of restenosis is <10%.
What happens after the angioplasty?
Following your angioplasty, the catheters will be removed, and a device will press on your wrist artery for a few hours, to allow it to heal. You will usually be kept overnight in the hospital and if you are well the next day, be allowed to go home.
You will be commenced on blood thinner tablets and be instructed on how long to take them. When you go home, drink plenty of fluids to allow the contrast dye to be flushed out of your system. You should avoid strenuous exercise for a few days and return to work a week after the procedure.
What are the risks of coronary angiography?
This is an invasive test of the heart and blood vessels, so there are some risks, luckily major complications are rare. The main risks are:
- Bleeding from the access site
- Injury to the arteries
- Heart attack
- Stroke
- Allergic reactions to the contrast
- Radiation exposure
What are the risks of a coronary angioplasty?
Coronary angioplasty is riskier than coronary angiography because you are having balloons and wires put into your heart arteries. The risks of major complications are however still rare. The types of problems that can occur are the same as for coronary angiography.
Why not just do a balloon angioplasty without a stent?
This is the initial technique that was used, unfortunately, after 1 year around 50% of arteries are reblocked. Stents were developed to prevent this.
How do I prepare for a coronary angiogram?
Angiograms are usually elective (scheduled in advance). You will be given detailed guidance on how to prepare by your doctor, but in general:
- Fast before the angiogram – ie don’t eat or drink from the night before.
- If you are diabetic as your doctor what to do about your medication
- Ask your doctor which of your regular medications you need to take before the procedure.
Does cardiac catheterization hurt?
It can be a little painful having the local anesthetic injected at your wrist or groin, but its job is to numb the area to allow insertion of the catheters without any pain.
What is a coronary stent and who needs it?
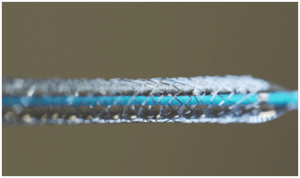
This is what a coronary stent looks like. It is used in most cases of coronary angioplasty.
How much does coronary angiography cost?
A coronary angiogram is just a diagnostic test of the heart arteries. It is usually done as a day case. The total cost is cheaper than angioplasty. The average total cost in private practice in Singapore is $4000 – $8000 SGD. Some insurance providers in Singapore may cover expenses on such procedures but be sure to talk with your provider first before undergoing such.
How much does coronary angioplasty cost?
The cost of coronary angioplasty is made up of a number of components: Cost of hospital stay; cardiologist fee; price of stents; cost of consumables and medications. In private practice, the average cost of coronary angioplasty and stenting is $40000 – $60000 SGD.
Recommended Reading: The Benefits of Choosing Allianz Insurance in Singapore for Cardiac Care
What is the best stent?
There is no “best stent”. Most modern stents have a special coating that helps prevent restenosis. These are called DES or drug-eluting stents. The choice of stent will often be driven by the type of blockage you have.
How long do stents last?
Stents are metal and stay in the body forever. Over time they get covered with your own cells and they basically become part of the arterial wall.
Are there alternatives to stents?
Yes, there are. The decision on what to do will be made after a full assessment and discussion with your cardiologist. The 3 main options are:
- Tablets only
- Coronary angioplasty and stenting
- Coronary artery bypass grafting
Are stents better than bypass surgery?
No technique can be said to be better than the other, they are both useful in different scenarios. Coronary artery bypass grafting surgery is often used when a patient has multiple blockages or is a diabetic; or if the type of coronary blockages is not amenable to stenting. CABG surgery is a very safe and effective strategy for blockages in certain patients and has excellent long-term results.
What is bypass surgery?
Coronary artery bypass grafting surgery (CABG) is open heart surgery. Your chest is opened, and arteries or veins are used to “bypass” the blockages by connecting them from the aorta to an area on the coronary artery after the blockage.
It is a big operation, that requires a general anesthetic and during the operation, the work of your heart and lungs is taken over by a heart-lung bypass machine.
You will usually be in the hospital for 5-7 days after the operation and take 6 weeks to 3 months to fully recover. Clinical trials have shown that in certain groups of patients it provides excellent long-term results.
Once I have a stent am I cured?
Angioplasty is not a cure! Once you have had your blockage opened with angioplasty the blood supply to the heart will be better and your symptoms should improve, however you still have coronary artery disease!
The process that led to coronary artery disease has not been fixed. Therefore lifestyle and medication are critical after you have had an angioplasty, and arguably they are more important than having a stent.
The correct lifestyle changes and medication will help prevent the worsening of disease AND more importantly reduce your risk of heart attacks and strokes.
- Stop smoking! The single most important thing you can do.
- Nutrition – stick to a Mediterranean style of eating. It has been shown to reduce the risk of heart attack and death.
- Lose weight
- Exercise at least 5 days per week.
- Ensure you blood pressure, cholesterol and blood sugars are checked regularly and are under control.
- Take all the medication you are prescribed.
I hope you have found this article useful. I am always available for advice if you have any concerns, just give me a call or send me an email.
Book an appointment with heart doctor in Singapore.
Related article: How Much Does It Cost To See A Cardiologist In Singapore?